What Are Pressure Injuries?
Pressure injuries, also called “bedsores” or “pressure ulcers,” are injuries to the skin and the tissues beneath. They develop over bony areas when someone stays in one position for too long. The constant forces of pressure, friction, and shear reduces blood flow to the area, which then cause the skin and the tissues to deform and break down.
Pressure injuries can be painful, take a long time to heal, disrupt sleep, affect mood, limit mobility, and reduce the quality of life for the affected individual. These injuries can also lead to infections, and in severe cases, even death.
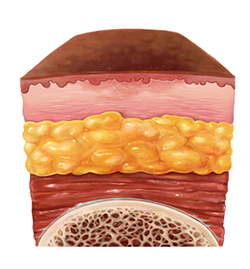
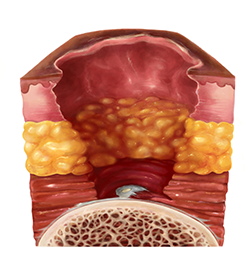
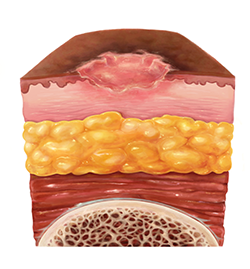
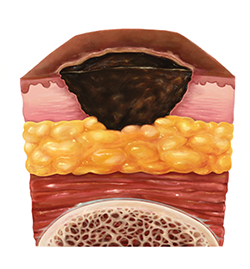
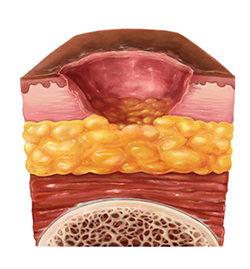
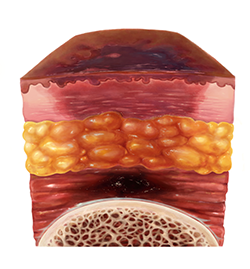
Pressure Injury Stages
You can find more information on recognizing these signs and symptoms here:
Strategies for Preventing Pressure Injuries
Keep the Pressure Off
Ensure the person in your care changes positions regularly. When lying down, reposition every 1-2 hours, and for those in wheelchairs, reposition every 15 minutes. To reposition, use a rolling action instead of a dragging motion to minimize friction and shear.
Keep the Skin Clean and Dry
Exposure to moisture from urine, feces, and sweat softens the skin, increasing the risk of skin damage. To keep the skin dry, replace soiled incontinence briefs (i.e., diapers) as soon as possible. Consider using skin barrier creams for added moisture protection.
Maintain Proper Nutrition
Promote healing by ensuring your loved one stays hydrated and eats enough calories, vitamins, minerals, and proteins. A well-nourished body has the energy to build new tissue, aiding in the healing of pressure injuries. Inadequate nutrition may lead to the breakdown of healthy tissue, such as muscle, slowing down the healing process and potentially causing the loss of muscle. Good nutrition also supports a stronger immune system, which is needed to help fight off infection.
Use a Specialty Mattress
Different mattresses, including ones made of foam and those with special air cells, are designed to prevent pressure injuries. Speak to your healthcare provider such as your Occupational Therapist for guidance. If you don’t have an Occupational Therapist, consider being referred to one.
Use Pillows and Padding
Use pillows and padding to offload pressure, which is done by minimizing or removing weight from the body. You can use sheepskin or foam for additional heel cushioning, elevate legs with pillows to raise the heels, and avoid donut-shaped cushions as these spread the pressure outwards. When the person in your care is in a wheelchair, pad the pedals to reduce heel pressure and ensure knees don’t rest against the bar.
Do Not Elevate the Head of the Bed More Than 30 Degrees
When the person you’re caring for is sitting in bed, avoid elevating their head too much to prevent sliding and shear, which can lead to the breakdown of skin and the development of pressure injuries in the lower back area.
When To Call a Doctor
If you notice a pressure injury, especially if your loved one has developed a blister or a sore, call your primary health care provider (doctor or nurse practitioner) immediately. Pressure injuries can advance quickly, and it is important to prevent the pressure injury from progressing any further.
Call your provider immediately if there are any signs of infection, such as:
- An unpleasant odor coming from the pressure injury
- Pus, or discharge, coming out of the pressure injury
- Red and tender skin surrounding the pressure injury
- The skin next to the pressure injury is swollen
- Fever
You may need to find a wound care nurse. Once you let your primary health provider know about the pressure injury, ask them to make a referral to a wound care nurse. A wound care nurse will be able to provide specific care, and will know which dressings to use on the pressure injury. They will also know how often the dressings must be changed.
It is normal to feel overwhelmed. Taking care of a pressure injury is difficult and its care can benefit from the help of a team. You may want to look into finding the following healthcare professionals to help manage the pressure injury: